Treating Perthes
Perthes disease is a highly variable and relatively uncommon condition so it is best treated by a pediatric orthopaedic surgeon who has the clinical interest and expertise treating Perthes.
It is important to discuss specific questions with your surgeon. Please note that the treatments discussed in this section are generalizations and not all treatments mentioned are appropriate for every patient.
How are treatment protocols chosen?
In general, treatment decisions are based on the age at the onset of the disease, the stage of Perthes that the patient is currently in, the amount of femoral head that is involved, and patient’s symptoms and loss of hip motion. Common goals of treatment include relieving pain, restoring hip motion, and preventing or minimizing deformity of the femoral head.
What are treatment options?
Treatment options vary based on the age of the patient and stage of disease. Nonsurgical options as well as surgical repair and treatment may be suggested over the course of the disease process. The primary goal of all treatment options are “containment” and maintaining or increasing range of motion.
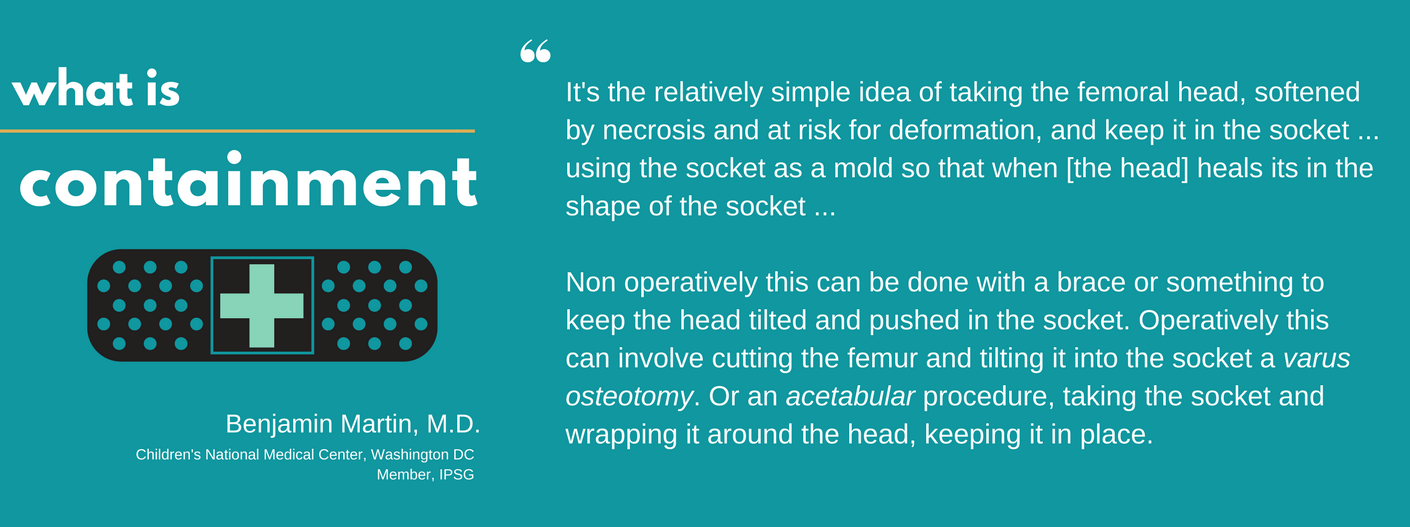
Non-operative Treatments:
-
Pain control: take analgesic (like Tylenol) or anti-inflammatory medications (like Motrin or Naprosyn) if needed for short time (few days)
-
Activity restrictions: avoid running, jumping, long walks, and sports
-
Crutches or walker: minimize pressure on hip while walking
-
Wheelchair: takes the pressure off the hip
-
Physical therapy: maintain hip motion and flexibility
-
Traction: improve motion and flexibility and decrease pain
-
Casts and braces: help to improve motion and keep the ball positioned in the socket
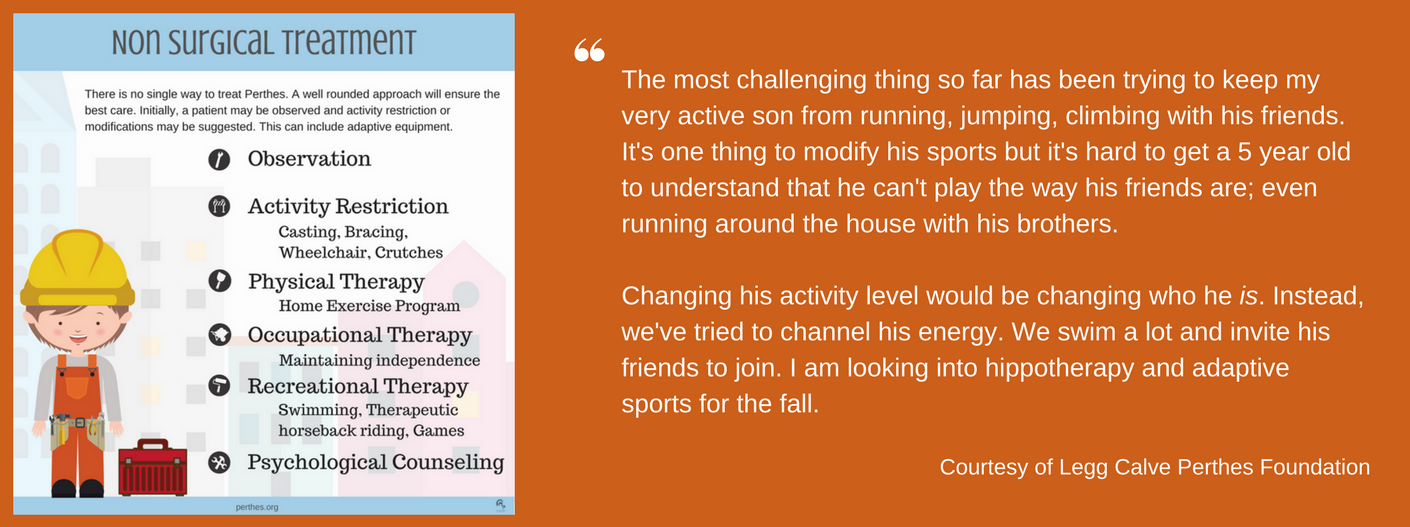
Surgical Interventions
Children may benefit from surgery to keep the ball in the socket and improve the chances of achieving a more round ball as the bone regrows. Conventional procedures include:
- Adductor tendon release – A tight groin muscle is surgically released to increase the hip motion (abduction) and allow the ball to be put into the socket. Petrie casts are placed to hold the hip in this position.
- Osteotomy – femoral, pelvic, or both bones of the hip are cut surgically for re-orientation. This will allow the ball to be better covered by the socket. This may help the ball regrow into a more round in shape.
New Treatments
It is important to note that newer treatments offer potential benefit of improving bone healing but they do not have the track record yet and they have not been researched to the same extent as the conventional treatments described above.
Hip distraction – Pins are temporarily placed through the skin into the pelvic and the femur bone to increase the space between the ball and socket (i.e. distraction or pull apart slightly). The increased space reduces pressure on the ball and decreases the chance of the ball healing with a flattened shape. This procedure is also known as hip arthrodiastasis.
Core decompression is a treatment used in adult avascular necrosis in which a hole is drilled into the femoral head and the dead bone is removed. Drilling this hole is thought to relieve pressure inside the femoral head to help alleviate pain. It also provides a potential new pathway for new blood vessels and healing cells to enter the femoral head. Core decompression has been utilized successfully in adults with early stage avascular necrosis of the hip before femoral head deformity occurs. Multiple epiphyseal drilling and femoral neck tunneling are variation of this concept of providing new pathway for new blood vessels and healing cells to enter the femroal head. In multiple epiphyseal, many small holes are made instead of one large hole to increase the number of pathways. The holes can be targeted to the area of femoral head that is most affected on MRI.
Bone marrow aspirate concentrate (BMAC) injection involves taking a child’s own bone marrow cells which are then concentrated by removing some cells (the plasma and red cells). The remaining cells are injected into the femoral head through a core decompression. The injected cells potentially differentiate into blood cells, bone cells, and fibrous cells which may speed up the healing process.
Experimental Treatments
Pharmaceutical
Bisphosphonates are medications that slow down bone loss and are used frequently in the treatment of osteoporosis. Investigators are trying to determine if bisphosphonates, either taken by mouth, intravenously (IV) or by direct injection into the femoral head will slow down femoral head collapse in Perthes disease and lead to a better long-term outcome. This treatment is considered experimental at this time. IPSG is planning to perform a clincial study using bisphosphonate in the future.
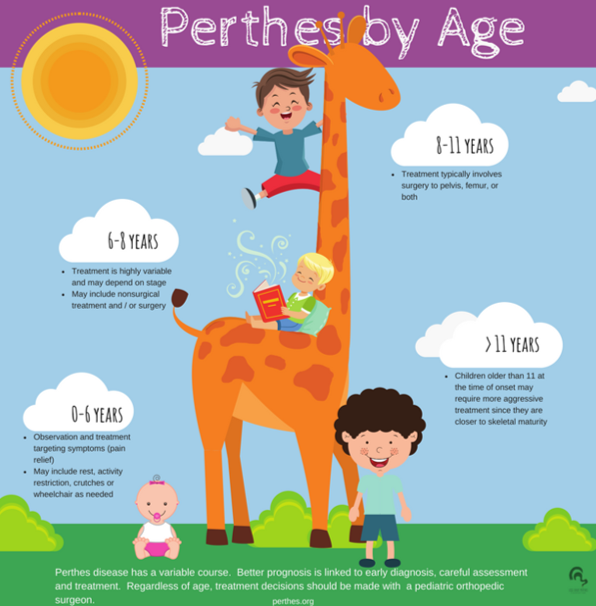
Treatment by Age
Since bone healing and regrowth potentials change with age, children that develop Perthes at a certain age should receive treatment appropriate to their age group and treatments on this site are described based on the age of the child. For example, younger children have more healing potential and more time to regrow their bone than older kids and may need less aggressive treatment.
Additionally, children with less area of the femoral head affected by the loss of blood flow have less diseased bone to heal than kids with more severe cases. Following are our current consensus on treatment by age. More detailed information is provided in each age group section below. There may be instances for each age group where a treatment more commonly used in other age groups may be recommended.
Under Age 6
Most children who are diagnosed with Perthes disease before the age of 6 have a favorable long term outcome regardless of the treatment. Most doctors recommend some activity restrictions, avoiding impact activities like running and jumping, while still allowing biking and swimming. Sometimes physical therapy is recommended to help with stretching and to minimize muscle weakness. Anti-inflammatory drugs may be used occasionally to help decrease pain in the hip. However, daily use of an anti-inflammatory drug may hinder bone formation.
 Wheelchairs and temporary bed rest may also be used to rest the hip. In hips that are very stiff or have more serious involvement, surgery may be recommended. Often it involves injecting dye into the hip, hip arthrography, and then moving the hip while looking at it with an x-ray machine when the kids are under anesthesia. Cutting of a tight tendon in the groin, also known as a tenotomy, followed by placing two casts with a bar between them in the shape of an “A”, or Petrie casts, shown here, helps to increase hip joint mobility and decrease inflammation. In rare cases, cutting the bones to reposition the hip is utilized.
Wheelchairs and temporary bed rest may also be used to rest the hip. In hips that are very stiff or have more serious involvement, surgery may be recommended. Often it involves injecting dye into the hip, hip arthrography, and then moving the hip while looking at it with an x-ray machine when the kids are under anesthesia. Cutting of a tight tendon in the groin, also known as a tenotomy, followed by placing two casts with a bar between them in the shape of an “A”, or Petrie casts, shown here, helps to increase hip joint mobility and decrease inflammation. In rare cases, cutting the bones to reposition the hip is utilized.
Age 6-8
This age group has the largest variability in treatment options. This age group also has the greatest variability in long term outcome with some kids doing very well and others developing degenerative arthritis. Some kids will have milder cases of Perthes that can be treated with activity restrictions, physical therapy and anti-inflammatory medication. Temporary bed rest or decreased weight bearing with a wheelchair or crutches can also be used to decrease the pressure on the hip and the hip joint irritation.
In more moderate cases with a very stiff hip, soft tissue surgery to increase hip joint mobility and casting to rest the hip are recommended. The surgery may involve injecting dye into the hip joint and then moving the hip while looking at it with an x-ray machine, arthrogram. Cutting of a tight tendon in the groin, also known as a hip adductor tenotomy, followed by placing a Petrie cast helps to increase leg spreading (i.e. hip abduction) and decrease inflammation. These Petrie casts are commonly worn for 6 weeks and then followed with a brace called A-frame that keeps the legs spread apart but allows kids to walk with assistance.
Unfortunately, many kids in this age group have more severe involvement and benefit from more extensive surgery. An osteotomy involves cutting one of the bones around the hip. This allows the hip to be repositioned for optimum healing. A femoral osteotomy means the cut is in the thigh bone and a pelvic osteotomy means the cut is in the socket bone above the hip. Both surgeries are meant to put the hip in a better position to get rounder healing of the ball joint. Plates and screws are commonly used to hold the cut bones and cast may be placed to protect the surgery. Physical therapy after surgery may be used to strengthen the muscles and maintain mobility. The plates and screws are routinely removed once the hip is healed.
Age 8 and Over
Kids diagnosed with Perthes after age 8 have the most guarded long term outlook. The natural history, or what would happen if nothing is done, is generally poor unless the disease is mild. Therefore surgery is frequently recommended.
Surgical treatment involves cutting one of the bones around the hip, and is called an osteotomy. A femoral osteotomy (shown) means the cut is in the thigh bone (also called femur) and a pelvic osteotomy means the cut is in the socket bone above the hip. Both surgeries are meant to put the hip in a better position to promote round healing of the ball joint. Plates and screws are commonly used to hold the cut bones and casts are placed to protect the surgery. 
Physical therapy after surgery may be used to strengthen the muscles and maintain mobility. The plates and screws are routinely removed once the hip is healed. Some cases are so severe that simply cutting the bones does not allow the hip to be repositioned.
A device outside the skin with pins connected to the thigh and socket bone can be used to help pull the bones apart and then allow them to be repositioned for the best fit. This is called a hip joint distraction with an external fixator. The external fixator may have hinges to allow some hip movement or may be solid not allowing movement. The external fixator is gradually adjusted until the hip is in the best position possible. The hip is then left in this “best fit” position for about 4 months to allow for healing. Physical therapy during the healing process and after the fixator is removed are very important. Some surgeons recommend doing the hip joint distraction surgery early to protect the ball part of the hip joint. Usual duration of hip joint distraction is about 3-4 months.
Alternative options of treatment, such as multiple epiphyseal drilling or femoral head tunneling are also being tried at some centers. However, the effectiveness of hip joint distraction and multiple epiphyseal drilling is not established and is being studied by the IPSG.